 |
| ----------------------------- SPECIAL REPORT ------------------------------ |
Despite our efforts and best wishes, our modus vivendi, work atmosphere and environment often lead to situations where we have to consult medics and get treatment. The Country Cooperation Strategy brief of the World Health Organization (WHO) informs that India accounts for 21 percent of the world’s global burden of disease.
The country is losing more than 6 percent of its gross domestic product (GDP) every year owing to premature deaths and preventable illnesses.
Among other things, recent reports, research papers and publications convey that rising out-of-pocket health expenditure (OOPHE) and failure of government-sponsored health insurance schemes have put enormous financial burden on especially the poor.
The Twelfth Five Year Plan (2012-2017) document earlier noted that the lack of extensive and adequately-funded public health services compel most people to incur heavy out-of-pocket expenditures on services purchased from the private sector. A large fraction of the OOPHE arises from outpatient care and purchase of medicines, which are mostly not covered by the existing insurance schemes, thus, leading to impoverishment amongst people.
As per the International Labour Oraganization's World Social Protection Report 2014-15, during 2011 nearly 60 percent of total (public and private) healthcare expenditure was financed by private households' out-of-pocket payments in India as compared to 35 percent and 15 percent in case of China and Bhutan respectively.
It could be seen that the provisional month-on-month annual rate of inflation in Consumer Price Index (Base 2012=100) of health has been higher in the rural areas (6.53 percent) as compared to urban areas (4.04 percent) as well as all-India combined (5.59 percent) during July 2015 (over July 2014). This means that inflation in retail prices of health services puts additional burden on rural consumers vis-à-vis the urban ones.
Budgetary allocation on health
The priority accorded to a particular sector by the government is judged by how much financial and fiscal support it provides to the concerned sector.
A recent opinion piece published in The Hindu Business Line by Indranil Mukhopadhyay reveals that government spending (which includes both Centre and states) on health as a percentage of GDP is just a little above 1 percent. Even governments of Afghanistan and Myanmar declare a better health budget than ours.
When price inflation is taken into consideration, it can be seen that in real terms both health allocation and expenditure have declined during the recent years in India. The Central Government’s expenditure on health as a percentage of GDP has become the lowest in the last four decades. Mukhopadhyay calculated that the Centre's spending on health as a percentage of GDP has actually worsened from 0.33 percent in 2009-10 to 0.23 percent in 2015-16.
Following the 14th Finance Commission recommendations, there has been a trimming down of finance available under the Central Sponsored Schemes, on the pretext that the share of states in total taxes has been raised. This has actually affected the implementation of National Health Mission (NHM), points out Mukhopadhyay.
It is also worth noting that during the Union Budget 2015-16, the sharing pattern of finance between the Centre and states for schemes such as the NHM and National AIDS and STD Control Programme (among 24 such schemes) have been changed.
Several other literature – such as Lant Pritchett & Gulzar Natarajan’s piece in The Indian Express or the paper An Estimate of Public Expenditure on Health in India (2012) by economists Mita Choudhury and HK Amar Nath from National Institute of Public Finance and Policy (NIPFP) – present evidence of the progressively diminishing budgetary allocation on health.
Public spending on health: The ideal deal
Based on recommendations of the High Level Expert Group (HLEG), the Twelfth Five Year Plan (FYP) adopted the strategy of rolling out the Universal Health Coverage (UHC). The Twelfth FYP envisaged that each individual would have assured access to a defined essential range of medicines and treatment at an affordable price, which should be entirely free for a large percentage of the population.
Among other things, the High Level Expert Group on UHC had recommended that public expenditure on health should be increased from 1.2 percent of GDP to at least 2.5 per cent by the end of the Twelfth FYP, and to at least 3 percent of GDP by 2022.
The Draft National Health Policy 2015 (published in December 2014) also proposes to raise public health expenditure to 2.5 percent of the GDP. It notes that 40 percent of this would need to come from Central government expenditure.
However, health activists argue that despite the promise of UHC, in real terms the allocation to and expenditure on health sector had actually been reduced in the first two years of Twelfth FYP.
NSS 68th round report findings
The 68th round National Sample Survey (NSS) Report entitled Level and Pattern of Consumer Expenditure 2011-12 informs that although an average urbanite spends nearly 84 percent higher than his/her rural counterpart every month, the share of total outlay on medical expense is higher for the latter (i.e. 6.7 percent) as compared to the former (i.e. 5.5 percent).
The NSS data indicates that rural elites spend a significantly larger portion of their outlays on health as compared to the urban ones.
71st round NSS: Recent trends
A recently published report on health based on the 71st round of NSS, titled Key Indicators of Social Consumption in India: Health, shows that in more than 70 percent ailment spells or cases which requires non-hospitalised treatment, Indians consult or rely upon the private sector (private doctors, nursing homes, private hospitals, charitable institutions etc).
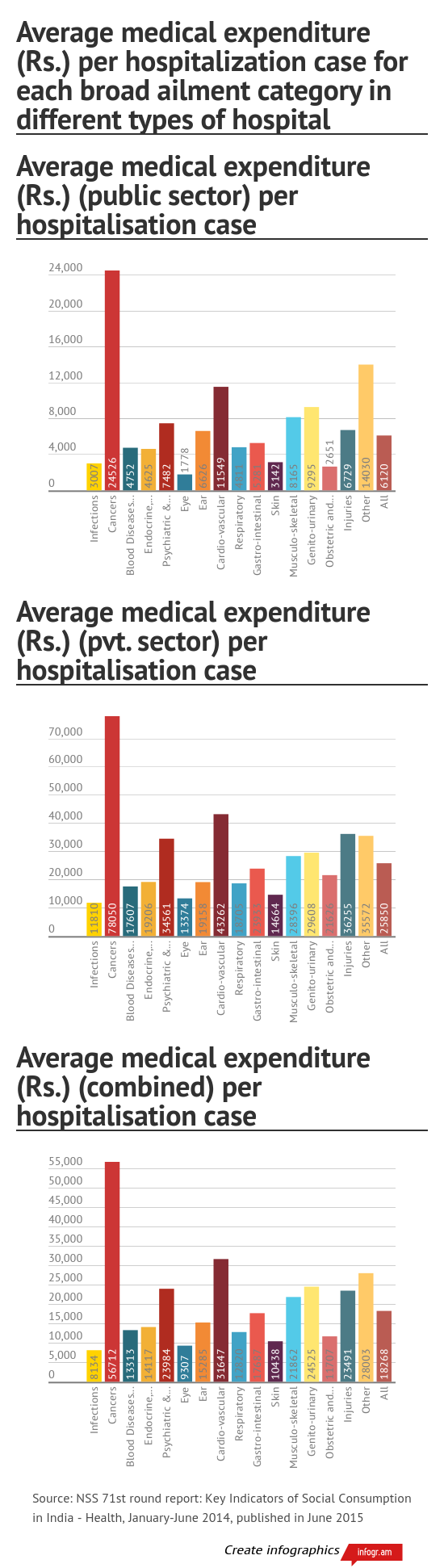
The NSS 71st round survey, which collected information from 36,480 households in rural areas and 29,452 households in urban areas, was conducted during January to June 2014. Among other things, it has found that the average medical expenditure per hospitalisation in private hospitals is roughly four times higher as compared to that in public hospitals.
Despite that, data reveals that 68 percent of hospitalised treatment is carried out in private hospitals in urban areas, as compared to 58 percent in rural areas.
Also, in both rural and urban areas, the poorer households rely more on the public sector for hospitalised treatment than the better-off sections of the population.
The NSS report mentions that a majority of the population in India i.e. close to 86 percent of rural population and 82 percent of urban population are not covered under any scheme of health expenditure support. Health expenditure coverage is broadly correlated with levels of living in both rural and urban areas.
In rural areas, around 13 percent of the population is covered under government funded insurance schemes such as Rashtriya Swasthya Bima Yojana (RSBY) or similar plans, whereas in urban areas this figure is 12 percent.
In the urban areas, nearly 4 percent of the population on their own have taken health insurance from a company, whereas in rural areas this figure is almost negligible.
Close to 2 percent of urban population is supported by health protection given by their employers, whereas less than a percentage of rural population is supported by the same.
Only 6 percent of expenditure made on hospitalised treatment is reimbursed partly or fully in urban areas whereas a meagre 1 percent is reimbursed in rural areas.
For meeting, medical expenditure during hospitalisation, roughly a quarter of rural households depend on borrowings as against a little less than one-fifth of urban households.
The average total medical expenditure for non-hospitalised treatment per ailing person in urban areas is about 26 percent higher than in rural areas.
For each hospitalisation case, the medical expenditure of the top 20 percent of the rural population (in terms of Usual Monthly Per Capita Expenditure or UMPCE) is roughly double that of the bottom 20 percent during the stay at hospital. In contrast, the medical expenditure of the top 20 percent of the urbanites is almost 4 times that of the bottom 20 percent. UMPCE for a household is the household’s usual consumer expenditure in a month divided by the household size.
For non-hospitalised treatment, the medical expenditure of the top 20 percent of the rural population (in terms of UMPCE) is roughly 18 percent higher than the bottom 20 percent; For urbanites, the medical expenditure of the top 20 percent is almost 75 percent higher than the bottom 20 percent.
Rising burden of OOPHE on the poor & disadvantaged
Several studies point to the burden on the population due to the rise in their share of OOPHE in total consumption expenditure, especially on the poorer and marginalised sections.
A 2015 working paper by economists Indrani Gupta and Samik Chowdhury from the Institute of Economic Growth (Delhi) reveals that between 1993-94 and 2011-12 the have-nots experienced greater increment in real OOPHE on diagnostics and other miscellaneous expenses as compared to the better-offs.
For both inpatient (institutional, which require hospitalisation) and outpatient treatment (non-institutional), expenditure on medicines forms a major part of total expenditure. While the share of medicines in total health expenditure has declined over the years, a rise in the share of almost all other components could be noticed during the same span.
Gupta and Chowdhury observe that the sharpest increase in the share happened in the case of diagnostics. The share of diagnostics in OOPHE more than doubled between 1993–94 and 2011–12 for both inpatient and outpatient services.
The share of other miscellaneous expenses for inpatients, which includes expenditure on transport, lodging, food and miscellaneous expenditures of the ailing and her escort(s) etc., also exhibited a rising trend.
In the same period, the per capita real consumption increased annually by 1.9 percent, while per capita real OOPHE grew every year by 4.1 percent. As a whole, the share of OOPHE in total household consumption expenditure has increased from 4.9 percent in 1993-94 to 6 percent in 2004-05, and further to 7.2 percent in 2011-12.
Between 2004-05 and 2011-12, the rise in per capita real OOPHE was highest for the poorest 20 percent of the population as compared to other income/ expenditure classes, according to the IEG working paper.
Yet another 2014 study by Anup Karan, Sakthivel Selvaraj and Ajay Mahal, which was published in the prestigious PLOS One journal, shows that the share of OOPHE in total household expenditure increased sharply among Muslims (relative to non-Muslims) during the period 1999-2000 to 2011-12.
Similarly, OOPHE rose as a share of total household spending faster for Scheduled Caste/ Scheduled Tribe households relative to non-SC/ST households.
Government schemes: Where are the loopholes?
Among other things, it has been found by the Draft National Health Policy (NHP) 2015 that states with better capacity at the baseline were able to take advantage of the financing under National Rural Health Mission (NRHM) sooner, while high focus states had to first revive or expand their nursing and medical schools and revitalise their management systems.
The larger gaps in baselines and the longer time needed to develop capacity to absorb the funds actually worsened the gaps between the desired norms and actual levels of achievement in these high focus states. Inefficiencies in fund utilization, poor governance and leakages became valid concerns in some of the weaker states.
Under the NRHM, not much attention was given to action on social determinants of health, notes the Draft NHP 2015.
The low awareness among the beneficiaries about the entitlement and how and when to use the RSBY card are major problems of the government funded insurance scheme. Denial of services by private hospitals for many categories of illnesses and over supply of some services have also been noticed under the RSBY. The Draft NHP 2015 mentions that some hospitals, insurance companies and administrators resort to various fraudulent measures, including charging informal payments.
The study by Anup Karan et al published in PLOS One shows that central programmes like NRHM and RSBY, as well as state-level initiatives (such as those in Karnataka, Andhra Pradesh, Tamil Nadu) could do little to reduce the financial burden arising out of personal expenses on healthcare, especially for India's poorest and underprivileged social and religious groups.
According to the study, the following factors primarily contributed to rising personal health expenses:
a. The focus of the NRHM shifted largely to reproductive and child health (RCH) interventions. Thus, relative neglect of primary care led to increased financial burden on poor and other less advantaged population groups.
b. Only a few state governments provided access to subsidized drugs as a result of which households have been forced to pay for medicines from their own pocket.
c. Publicly-financed insurance schemes may facilitate healthcare, but they may also lead to additional (out-of-pocket) contributions due to limited financial cover, especially if the demand for health service use exceeds the approved upper limit for coverage and also because coverage of post-hospitalisation care is limited.
d. Healthcare provision and financing innovations are possibly poorly targeted. The BPL list prepared by various states suffers from a high degree of ‘exclusion' and ‘inclusion’ errors. Existing literature suggests that SC/ST populations tend to benefit less from public programmes than other population sub-groups.
To conclude, therefore, the citizenry faces a precarious situation where on one hand, the allocation and expenditure on public health is getting curtailed, and on the other hand, the existing programmes and insurance schemes of the government are failing to curb the growing OOPHE of especially the poor.
As mentioned in the Draft NHP 2015, India surely needs a Right to Health legislation of its own like Brazil and Thailand. Increasing the public spending on health to 2.5 percent of country’s GDP is essential to stop the rising burden of OOPHE. But the Draft NHP 2015 itself has been subject to criticism for promoting corporatization of the health sector, which gives more space to the private sector and health industry.
It is high time for the government to start looking for best practices on access to health, which are affordable and sustainable. This probably is every citizen’s ‘mann-ki-baat’ today. A ‘one-size fits all’ model of healthcare delivery is unlikely to work in a complex country like ours.

No comments:
Post a Comment